Abstract
Introduction
The use of prescribed medications has risen dramatically in the past decades.1 In 2008, over 76% of Americans older than 60 years reported ingesting two or more prescribed medications daily, and 37% used five or more.1 Patients who use indicated medications appropriately can expect to derive benefit. Yet, a significant proportion will experience adverse drug events, the unintended and harmful effects resulting from medication use that are associated with suboptimal patient outcomes and increased health services utilization.2-7 Adverse drug reactions alone, a subset of adverse drug events that occur when drugs are used in therapeutic doses,8 cause 5-10% of acute care hospital admissions,9-12 prolong hospital stays,13 and may contribute to more potential years of life lost than all other injuries combined.14 Efforts to optimize medication use and reduce adverse drug events are therefore a public health priority.15
- Myocardial infarction in women without obstructive coronary artery disease
- Peptic Ulcer – Symptoms, Diagnosis, and Assigning the Correct ICD-10 Codes
- SUDAFED® Sinus 12 Hour Pressure + Pain Relief Decongestant Caplets
- Extraction Facials: Blackhead Extraction, Milia, Pore & Pimple Extraction
- Spring Valley Hyaluronic Acid Serum, 2 Oz
Adverse drug events that are encountered in clinical practice may vary substantially from those observed in pre-market clinical trials.16 Reasons include differences in patient populations, treatment indications (eg, off-label use), monitoring protocols, duration of drug exposure and compliance between the clinical practice setting and the controlled environment of clinical trials.6,16,17 Monitoring and evaluating health outcomes that are associated with the way medications are used in clinical practice is difficult, yet essential to understanding the ongoing safety and risk-benefit profiles of medications, and paramount to promoting their optimal use.
Bạn đang xem: ICD-10 codes used to identify adverse drug events in administrative data: a systematic review
Administrative databases, electronic health records and disease registries contain a plethora of health data that can be used to ascertain health outcomes in clinical practice. These data are generally inexpensive, readily accessible and have been collected without interfering in the delivery of care. Thus, data from these sources are more likely to reflect the outcomes experienced by patients in the real-world clinical practice setting than the research setting, provided that the outcomes are appropriately identified and coded.16
Administrative databases worldwide, including in the USA, increasingly use the International Classification of Diseases (ICD) revision 10 system to classify diagnostic, health services utilization and death data. The ICD-10 coding dictionary enables coders to document adverse drug events in three ways: (1) by documenting the medication that caused an adverse drug event using ‘external injury cause codes’ (ie, Y40.0-59.9); (2) by documenting diagnoses that may be caused by a drug using ‘disease manifestation codes’ (eg, A04.7 Clostridium difficile colitis); and (3) by clustering an external injury cause code indicating the drug-related etiology with a disease manifestation code indicating the patient’s diagnosis.18 Because a large number of disease manifestation codes exist that might be adverse drug event related (eg, gastric ulcer), variation exists among health researchers in the code sets and coding algorithms used to identify adverse drug events coded in ICD-10.
Our main objective was to synthesize a comprehensive set of ICD-10 codes used by health researchers to identify adverse drug events. Our secondary objective was to identify studies with ICD-10 coding algorithms for adverse drug events.
Methods
Data sources and searches
This was a qualitative systematic review of the literature. Ethics approval was not required because it did not involve the use of human subjects or medical records.
A professional librarian (MDW) and study author (CMH) developed a systematic search strategy that was adapted for, and applied to, the following electronic bibliographic databases: MEDLINE (1948-2011), EMBASE (1980-2011), International Pharmaceutical Abstracts ((IPA) 1970-2011), Web of Science (1980-2011), the Cochrane Database of Systematic Reviews (1993-2011) and the Cochrane Central Register of Controlled Trials ((CENTRAL) 1996-2011) (see supplementary appendix A, available online only, for Medline search). Our search strategy combined three concepts: the ICD coding system, adverse drug events, and health outcomes. We reviewed the scope notes for each search term in order to identify and incorporate previous indexing terms, alternative keywords, and appropriate MeSH terms. No language filters were applied.
We hand-searched the following medical journals for relevant studies and conference proceedings from 2000 onwards: the Milbank Quarterly, Health Technology Assessment Journal, Health Affairs, Medical Care, American Journal of Medical Care, and Quality & Safety in Health Care. We used 2000 as the start date as this was the year that ICD-10 was introduced in Canada. We did not search for any additional conference proceedings not published in the above journals, as we thought it would be unlikely for code sets to be published in abstract format. We conducted an electronic grey literature search using the search engine Google with the same search terms that we used for our electronic bibliographic database searches. We hand-searched the bibliographies of all relevant articles. In 2012, we conducted periodic environmental scans of the literature for newly published studies using auto alerts from MEDLINE, EMBASE and IPA. We contacted content experts and authors of relevant studies for any additional studies and for clarifications about their methodology and code sets.
Study selection
We included all studies reporting the use of the ICD-10 coding system to identify adverse drug events in adult patients. Studies had to report the ICD-10 code set (our outcome measure) or coding algorithms used to search the administrative data. We excluded studies reporting only pediatric data, as common manifestations of adverse drug events vary between adults and children. In addition, pediatric adverse drug events are more commonly the result of dosing errors or unintentional toxic ingestions compared to adult adverse drug events. We also excluded studies using other coding systems, written in languages other than English, French and German, reporting only adverse events to illicit drugs or intentional overdoses, and studies that we could not access.
One study author (AK) screened all titles for potential eligibility using predefined criteria. Any potentially relevant studies were retained for abstract review. Two study authors (AK and CMH) reviewed the abstracts of potentially relevant titles. If either or both of the authors felt the abstract was potentially relevant, the full text article was retrieved and reviewed independently by two authors (AK and CMH) for inclusion and exclusion criteria. All disagreements about study eligibility at the full text review stage were resolved by achieving consensus through discussion.
Data extraction and quality assessment
Two authors (AK and CMH) independently abstracted data from included studies using standardized and piloted abstraction forms. Any disagreements over data abstraction points were resolved by achieving consensus through discussion, after contacting study authors for clarification. Data abstractors were not blinded to authorship or journal.
We are unaware of any validated quality assessment scales to measure the quality of non-comparator, retrospective population-based cohort studies.19 Therefore, we adapted relevant quality-assessment criteria from the GRACE guidelines and the York Centre for Dissemination and Reviews that were intended for population-based comparative effectiveness studies and reviews of adverse effects (table 1).19,20
Data synthesis and analysis
Xem thêm : Urinalysis for Pets: How At-Home Urine Testing Can Benefit Your Pet’s Health
We synthesized the data in a qualitative manner, with two authors (CMH and AK) reviewing all data extraction forms and re-reading primary manuscripts. A third author reviewed all tables and figures for accuracy (LR), and all authors subsequently critically reviewed the manuscript for content and accuracy. We adapted causality ratings for individual ICD-10 codes from two previous publications, and modified them by adding the rating ‘unlikely’ (U) for codes that other authors used to identify adverse drug events in the literature that we felt unlikely to have indicated an adverse drug event (table 2).21,22 We also added the rating ‘vaccine’ (V) for codes that were vaccine related. Two study authors (CMH and JS) independently, and blinded to one another’s ratings, assigned causality scores to ICD-10 codes without previously assigned causality ratings, and came to consensus through discussion about any disagreement.
Descriptive statistics were provided as averages with 95% CI, or medians with IQR. We calculated the interrater agreement of causality ratings assigned to ICD-10 codes, by collapsing causality ratings into a category indicating that an adverse drug event was very likely (categories A1, A2, B1, B2 and C), and a category in which adverse drugs events were deemed unlikely (categories D, E, U and V) based on the previous literature.21,22 We calculated κ scores with 95% CI as a measure of agreement beyond chance alone.
Results
Study characteristics and study quality
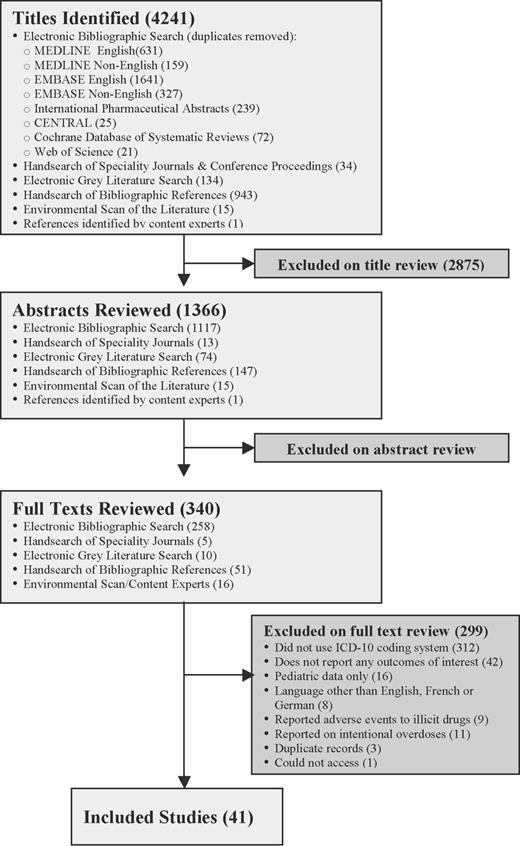
Our search revealed 4241 titles, of which 41 met our inclusion and exclusion criteria (figure 1). Sixteen studies were conducted in Europe,21-36 13 in North America,14,37-48 nine in Australia,49-57 and three in Asia (tables 3 and 4).58-60 The majority of included studies were non-comparator retrospective studies that used administrative data to ascertain the prevalence of adverse drug events in population-based cohorts. Twenty-eight studies examined adverse drug events in general as the main outcome measure,14,21-26,29,32-40,42,43,49-54,56-58 and 13 examined drug or drug class-specific adverse drug events.27,28,30,31,41,44-48,55,59,60 Eleven of 28 studies reported explicit methods for identifying the ICD-10 code set they used.21-23,34-36,38,40,42,53,58
We found a total of 827 individual ICD-10 codes that have been used in the health literature to identify adverse drug events (see supplementary appendix B, available online only, for the complete list of codes). Of these, 175 were external injury cause codes (Y40.0-59.9), and 652 disease manifestation codes. Only 13 disease manifestation codes only appeared in combination with a clustered code (table 5).52,61 Among studies examining adverse drug events in general, the median number of codes used was 190 (IQR 156-289). Seven studies used the external injury cause codes Y40.0-59.9 only,25,26,39,51,54,56,57 five studies used disease manifestation codes only,23,24,32,33,37 and 16 studies used a combination of both types of codes.14,21,22,29,34-36,38,40,42,43,49,50,52,53,58 Only one guideline recommended the use of algorithms to search for clustered codes, specifying external injury cause codes that should be clustered with specific disease manifestation codes in order to identify known adverse drug events.52 This list of clustered codes can be accessed freely online.61 The most common disease manifestation codes used are listed in table 6. Two authors independently assigned causality ratings to each ICD-10 code that had not previously had a causality rating assigned. The κ statistic as a measure of interrater agreement was 0.88 (95% CI 0.78 to 0.97).
Among studies looking for drug or drug class-specific adverse events, all studies reported the entire code set they used. The median number of codes that was used was three (IQR 1.5-10) (table 4). One study used external injury cause codes only,44 six studies used disease manifestation codes only,28,30,31,46,47,59 and six studies used a combination of both types of codes without any requirement for the codes to be clustered.27,41,45,48,55,60
Quality assessments
Among the 28 studies looking at adverse drug events in general, 19 reported an explicit definition of their primary outcome measure that was independent of the ICD-10 code set.14,21,22,25,29,32,36-40,42,43,49,51,54,56-58 Of these, 9 reported definitions for adverse drug reactions,29,36,39,40,49,51,56,57,62 5 definitions for adverse drug events,14,21,22,38,58 and one explicit definitions for both.54 Three studies used death as a result of poisoning or prescription drug use as primary outcome.37,42,43 Among the 13 studies on drug or drug class-specific adverse events, all provided definitions for their primary outcome measure with 4 using drug-induced deaths41,44,45,47 and 4 hospital admission due to an adverse drug event.30,46,55,59
Among the 28 studies looking at adverse drug events in general, 11 provided methods for their selection of ICD-10 codes.21-23,34-36,38,40,42,53,58 Methods included searching the ICD-10 code dictionary for diagnoses that could be attributable to medications (ie, gastric ulcer) and/or phrases (ie, ‘drug-induced’), empiric study of existing pharmacovigilance reports and mapping of events to the ICD-10 code dictionary,21,22,53 and literature review.21,22,34-36 Others adopted code sets that had previously been established by other authors.23,38,40,58
Only two studies estimated the sensitivity with which their code set may have ascertained the desired outcomes.38,40 Wu et al40 compared records containing adverse drug event-related diagnoses between two administrative databases. The authors’ premise was that for patients admitted to hospital through the emergency department for a drug-related diagnosis, the emergency department discharge and hospital admitting diagnoses should be similar. Using an ICD-10 code set containing 245 drug-related codes, including the external injury cause codes, Wu et al40 found that 15% of drug-related emergency department visits leading to hospital admission were coded with a corresponding admitting diagnosis. Wu et al40 estimated the specificity of their code set, and found it to be 99.7%. In comparison, in a study including both admitted and discharged emergency department patients, in which adverse drug events were identified prospectively by pharmacists and physicians, 6.8% of prospectively identified adverse drug events were identifiable using an ICD-10 code set consisting of diagnoses rated as definitely, very likely or likely to be related to medications.38 When the code set was broadened to include lower likelihood codes, 28.1% were identifiable with little drop in the code set’s specificity (98.7-87.7%).
Three studies considered the uncertainty of the causal link between drug exposure and the adverse event, and provided analyses allowing the reader to ascertain the impact that this may have had on the study results.21,22,38
Discussion
Our objective was to synthesize a comprehensive set of ICD-10 codes and coding algorithms that have been used by health researchers to identify adverse drug events in administrative health data. Among 41 published studies, we found 827 ICD-10 codes that have been used for this purpose. There was a large degree of variability in the number and types of codes used between studies, and only one published guideline recommended the use of algorithms to identify external injury cause codes clustered with disease manifestation codes. Of the reviewed studies, two provided estimates of the code set’s sensitivity and specificity.
Adverse drug events represent a growing public health concern.3 In the USA, adverse drug events represent the fourth to sixth leading cause of death, and are a frequent cause of unplanned hospitalizations, emergency department visits and ambulatory care encounters.5,10,63-65 The focus of the US$1 billion federal private-public initiative, Partnership for Patients, is to reduce hospital-acquired conditions by 40% and hospital readmissions by 20% by the end of 2013.66
In order to accomplish this target, the Partnership for Patients has identified the reduction of in-hospital adverse drug events as a priority. One intervention that the Partnership for Patients is promoting to accomplish this goal is medication reconciliation, a health systems intervention aimed at decreasing adverse drug events that result from the inaccurate transfer of medication information.67,68 However, to date little research has been conducted to describe and rank possible etiologies of adverse drug events, and as a result, it is largely unknown to what extent inaccurate transfer of medication information contributes to the development of clinically significant adverse drug events. Thus, it is not surprising that a recent systematic review of 26 controlled studies failed to find an effect of medication reconciliation on downstream health services use, mortality or cost.69 This example underscores the need for further development of innovative, evidence-based and effective patient safety strategies to reduce adverse drug events, and for their evaluation on health outcomes before their implementation outside of the research setting.
In order to inform the development of strategies to reduce preventable adverse drug events, the burden of disease in different healthcare settings and patient populations and their common etiologies need to be understood. This will help to prioritize and rationalize the development and evaluation of emerging strategies to prevent commonly occurring events associated with health services use and cost. Modifiable risk factors that can be targeted in carefully designed health systems interventions need to be identified. These may be related to medications, medication classes, treatment protocols, prescribing patterns, patient groups, provider groups, healthcare settings, and models of care, some of which may assist in developing successful interventions. Once developed, strategies are likely to benefit from refinement to enhance their feasibility of implementation and their performance. Finally, their impact on health outcomes and cost must be evaluated and compared with that of other health interventions in order to guide rational resource allocation and optimize health value for expenditure.
Xem thêm : Spring Valley Hyaluronic Acid Serum, 2 Oz
Population-level administrative health data that can be linked with medication dispensing data may represent a rich source of health information for this type of work. Adverse drug event data from this source may offer accessible and standardized population-level data over long time periods, enabling analysis of time trends, prescribing patterns, and comparisons across healthcare settings.16,70 However, no consensus presently exists among health researchers on how to identify adverse drug events reliably within such data sources, leading to substantial variability in the methods used for their identification.
Our study is the first systematically to review the health literature to synthesize a comprehensive set of ICD-10 codes previously used to identify adverse drug events. Previous studies have identified code sets by relying on ad hoc reviews of the literature, and mapping of drug-related diagnoses and pharmacovigilance case reports to the ICD-10 code dictionary. Most have adopted and used code sets developed by previous authors without conducting any validation studies to understand their sensitivity or specificity. When examining the code sets, common manifestations of adverse drug events have often been omitted (eg, E16.2 hypoglycemia), while the codes of rare events are commonly used (eg, T88.3 malignant hyperthermia due to anesthesia). This is problematic, as multiple studies relied entirely on disease manifestation codes to identify drug-related diagnoses. The omission of common manifestations of adverse drug events from their code sets based on the assumption that they might be associated with low positive predictive values would probably have dramatically influenced the numbers and types of adverse drug events found.
There is general agreement among health researchers that adverse drug events are underreported in administrative data, and that the effect of coding quality on adverse drug event identification is poorly understood.23,34,38-40,71 Based on our review, it is also possible that the use of incomplete code sets for adverse drug events may be a contributing factor. We found only two studies that evaluated the sensitivity of their ICD-10 code sets for adverse drug events, and both were low.38,40 Therefore, validation of a more comprehensive set of adverse drug event-related ICD-10 codes is necessary to try and enhance the sensitivity of the code sets used, while retaining specificity. This work needs to be conducted in a variety of care settings (eg, hospital vs ambulatory care), on a variety of adverse drug event types (eg, adverse drug reactions vs non-adherence), on different grades of adverse drug event severity (eg, severe vs mild), and by syndrome (eg, intracerebral hemorrhage vs epistaxis). Different clinical practice settings may influence the diagnostic performance of the code set(s) that is/are used, and may require refinements of the code sets used. Finally, it may be that administrative data may be well suited to tracking and investigating some consistently coded and identifiable adverse outcomes (eg, bleeding events), but not all manifestations of drug-related events (eg, delirium). Thus, we cannot recommend the adoption of our proposed code set without validation and further refinement. Instead, we present a comprehensive list of codes that we hope will provide the basis for further investigation, debate and consensus building in this area.
Due to the multiple ways in which adverse drug events may be coded (ie, by using external injury cause codes only, disease manifestation codes only, clusters of codes, or a combination of these methods), methodologies need to be developed to avoid double counting. Two of the studies we reviewed concluded that double counting was indeed possible when searching for adverse drug events using a combination of external injury cause codes and disease manifestation codes, and that this occurred in up to 15% of records.35,36 Similarly, studies need to be conducted to understand to what extent the use of disease manifestation codes (ie, E87.1 hyponatremia), which may indicate an adverse drug event or a non-drug-related event, may influence the sensitivity and specificity of the code set. To date, only one study has compared the sensitivity and specificity of narrower and broader code sets, and compared them to an independent prospective criterion standard in emergency department administrative data.38 In that study, while the broader code set led to higher sensitivity (6.8% vs 28.1%), broadening the code set had little impact on the code sets’ specificity.38 Unfortunately, the study did not examine coding quality to determine which steps during the patient care and coding trajectory may have contributed most to the under-coding of adverse drug events. Finally, methods to identify and understand the extent to which adverse events related to prescription medication use may be coded using codes that do not distinguish between prescription drugs and drugs of abuse (eg, F11 mental and behavioral disorders due to the use of opioids) need to be developed.
The most widely used definition for adverse drug events is ‘harm caused by the use of a drug’.2,72 In this study, we presented all definitions as reported by the study authors, as these may have led to variability in the code sets used. The existing inconsistency in the operational definition of adverse drug events needs to be addressed before being able to achieve consensus on a common code set(s), and may enhance the consistency with which adverse drug events are identified and reported, and thus comparability between studies. Given this limitation, we provided a comprehensive list of definitions and a corresponding code set that may serve as a point of reference for consensus building.
We did not attempt to meta-analyze data on the prevalence of adverse drug events, as this was not the objective of our study. In addition, significant differences in the ICD-10 code sets used to find adverse drug events are likely to result in significant heterogeneity between studies, and any differences that are found may simply be due to the methods used to identify them.
Ongoing national adaptations of the ICD-10 coding systems have introduced additional variability in the coding of adverse drug events that we were unable to account for. Not all studies described explicitly which national adaptation and versions of the coding dictionary they based their code set on. Some adaptations, for example, the German modification, may use additional two-decimal subcategorizations of individual disease manifestation codes that allow more refined coding than other systems. At present, the USA only uses ICD-10 coding for mortality reporting, explaining why all the US studies reported only on events related to death. Thus, while the majority of code categories are comparable across coding systems, the variability between national adaptations and coding versions used needs to be taken into account before application of any code set.
Additional limitations of our work are that we only reviewed publications in English, French and German. We also did not search extensively for abstracts or conference proceedings, as we thought we would be unlikely to find code sets published in these formats. We applied the only causality rating system that we are aware of for adverse drug event-related ICD-10 codes.21,22 While the causality rating system is based on clinical reasoning, and therefore inherently subjective, it may provide health researchers with a framework with which to start incorporating the certainty/uncertainty of drug-related causes to diagnoses identified in ICD-10. Therefore, we applied the previously proposed causality categories to additional ICD-10 codes that we identified through our review.
In conclusion, in this study we have synthesized a set of ICD-10 codes that have been used by health researchers to identify adverse drug events in administrative health data. Our code provides a basis for future work in establishing comprehensive and agreed-upon code sets that can be validated and refined for future work in this area.
Contributors
All authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: CMH and JS. Acquisition of data: CMH, AK and LR. Analysis and interpretation of data: CMH and AK. Drafting of the manuscript: CMH. Critical revision of the manuscript for important intellectual content: All authors. Administrative, technical or material support: LR. Study supervision: CMH.
Competing interests
CMH is supported by a New Investigator Award from the Canadian Institutes of Health Research, and is a member of the Drug Safety and Effectiveness Network.
Provenance and peer review
Not commissioned; externally peer reviewed.
Data sharing statement
The ICD-10 code set is available from the authors.
References
Nguồn: https://vuihoctienghan.edu.vn
Danh mục: Info
This post was last modified on Tháng mười một 23, 2024 3:21 chiều