Head injury is a serious condition that requires immediate medical attention. Generally, a person suffering from a head injury may not initially experience any feelings of being sick, but bleeding can occur within the skull. Internal bleeding can lead to serious consequences, including severe brain damage and even death. One type of internal bleeding in the skull is called subdural hematoma. Also called a subdural hemorrhage, this condition occurs when a vein located below the skull ruptures and starts to bleed. The blood collects between the skull and the surface of the brain. As the volume of hematoma (blood clotting) increases, brain parenchyma gets compressed and displaced, and the intracranial pressure may rise and cause herniation, leading to unconsciousness and death. Subdural hematomas can be caused by minor accidents to the head, major trauma, or the spontaneous bursting of a blood vessel in the brain (aneurysm). Treatment for this head injury is generally based on the type and severity of the injury. Typically, surgery is recommended for most subdural hematomas. However, very small hematomas may be carefully monitored first to see if they heal without having an operation. Neurosurgeons or neurology specialists who provide appropriate treatment for this type of injuries should also ensure that the medical coding for this condition is properly done on the medical claims. Proper coding on the medical claims is crucial for medical coding companies to ensure accurate documentation and reimbursement.
Subdural hematoma can be either acute or chronic. Acute subdural hematoma is the most dangerous type usually caused by a vehicle accident, a blow to the head or a fall from a height. Such cases form quickly and are often harder to treat. It is estimated that the death from an acute subdural hematoma is more than 50 percent. Chronic subdural hematoma on the other hand, is caused by mild or repeated head injuries. These are more common among older adults who repeatedly fall and hit their heads.
Bạn đang xem: Documenting and Coding Subdural Hematoma – Know the ICD-10 Codes
Common Symptoms
The symptoms of subdural hematoma can depend on the type of injury (whether it’s acute or chronic) and can vary from one person to another. Symptoms of an acute subdural hematoma occur rapidly following an injury. In cases of chronic subdural hematoma, symptoms are more likely to develop slowly or may not develop at all. Common symptoms include –
- Severe headache
- Vision problems
- Slurred speech
- Seizures
- Mood swings
- Loss of consciousness or passing out
- Dizziness and vomiting
- Confusion
- Apathy and weakness
Other potential risk factors that could increase a person’s chances of developing subdural hemorrhage include – patient’s age, medical conditions (that cause blood clotting issues), long-term alcohol use or abuse, blood thinners (such as warfarin or aspirin) and repeated head injuries (such as from falls or sports).
How a Subdural Hematoma Is Diagnosed
Diagnosing subdural hematoma quickly is important so that the treatment programs can be initiated immediately. Timely treatment may help minimize the risk of severe complications or even death. In most cases, head hemorrhage is quite difficult to diagnose as certain types do not depict any specific symptoms quickly or may have not have an obvious cause.
As part of the initial diagnosis, physicians will conduct a thorough physical and neurological examination to check for blood pressure and pulse, reflexes and balance, vision (the way the eyes respond to light) and the patient’s ability to answer questions and remember things. Physicians will also ask several questions about – occurrence of any head injuries (past and present), pain symptoms developed, medications taken, medical health problems and alcohol or drug consumption habits.
Xem thêm : Abortion Pill Humphrey Nebraska
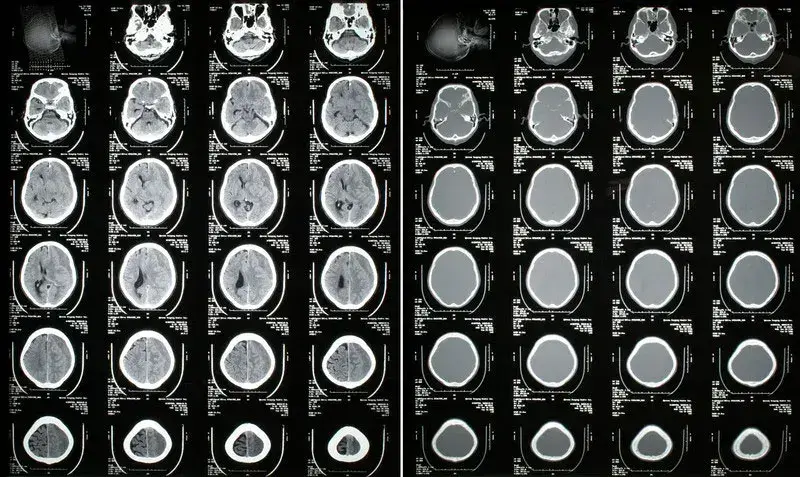
Several diagnostic tests like computed tomography (CT), or magnetic resonance imaging (MRI) scans will be conducted to get a clear picture of the different parts of the brain, skull, veins and other blood vessels and to check for any specific signs of blood clotting. If the physician identifies bleeding in any area, the source of the bleeding will be determined and a plan of action developed to address the specific issue. In addition, neurologists will also check your blood pressure and heart rate and recommend a detailed blood test to check for the total blood count. A complete blood count measures your red blood and white blood cell count and platelet count. A low level of red blood cells can indicate significant blood loss.
Treatment options for subdural hemorrhage may mainly depend on the type and severity of injury. Surgery will be recommended as the best option in most cases of subdural hemorrhage. Surgical techniques include craniotomy (a section of the skull is temporarily removed in order to access and remove the hematoma) and burr holes (a small hole is made in the skull and a tube is inserted through the hole to help drain blood clots). However, very small subdural hematomas may be carefully monitored first to see if they heal without having an operation.
Neurosurgery medical coding involves using the specific ICD-10 diagnosis codes for reporting subdural hematoma on the medical claims they submit to health insurers for reimbursement.
ICD-10 Codes to Use for “Subdural Hemorrhage”
S06.5 – Traumatic subdural hemorrhage S06.5X – Traumatic subdural hemorrhage S06.5X0 – Traumatic subdural hemorrhage without loss of consciousness
- S06.5X0A – Traumatic subdural hemorrhage without loss of consciousness, initial encounter
- S06.5X0D – Traumatic subdural hemorrhage without loss of consciousness, subsequent encounter
- S06.5X0S – Traumatic subdural hemorrhage without loss of consciousness, sequela
S06.5X1 – Traumatic subdural hemorrhage with loss of consciousness of 30 minutes or less
- S06.5X1A – Traumatic subdural hemorrhage with loss of consciousness of 30 minutes or less, initial encounter
- S06.5X1D – Traumatic subdural hemorrhage with loss of consciousness of 30 minutes or less, subsequent encounter
- S06.5X1S – Traumatic subdural hemorrhage with loss of consciousness of 30 minutes or less, sequela
S06.5X2 – Traumatic subdural hemorrhage with loss of consciousness of 31 minutes to 59 minutes
- S06.5X2A – Traumatic subdural hemorrhage with loss of consciousness of 31 minutes to 59 minutes, initial encounter
- S06.5X2D – Traumatic subdural hemorrhage with loss of consciousness of 31 minutes to 59 minutes, subsequent encounter
- S06.5X2S – Traumatic subdural hemorrhage with loss of consciousness of 31 minutes to 59 minutes, sequela
S06.5X3 – Traumatic subdural hemorrhage with loss of consciousness of 1 hour to 5 hours 59 minutes
- S06.5X3A – Traumatic subdural hemorrhage with loss of consciousness of 1 hour to 5 hours 59 minutes, initial encounter
- S06.5X3D – Traumatic subdural hemorrhage with loss of consciousness of 1 hour to 5 hours 59 minutes, subsequent encounter
- S06.5X3S – Traumatic subdural hemorrhage with loss of consciousness of 1 hour to 5 hours 59 minutes, sequela
S06.5X4 – Traumatic subdural hemorrhage with loss of consciousness of 6 hours to 24 hours
- S06.5X4A – Traumatic subdural hemorrhage with loss of consciousness of 6 hours to 24 hours, initial encounter
- S06.5X4D – Traumatic subdural hemorrhage with loss of consciousness of 6 hours to 24 hours, subsequent encounter
- S06.5X4S – Traumatic subdural hemorrhage with loss of consciousness of 6 hours to 24 hours, sequela
S06.5X5 – Traumatic subdural hemorrhage with loss of consciousness greater than 24 hours with return to pre-existing conscious level
- S06.5X5A – Traumatic subdural hemorrhage with loss of consciousness greater than 24 hours with return to pre-existing conscious level, initial encounter
- S06.5X5D – Traumatic subdural hemorrhage with loss of consciousness greater than 24 hours with return to pre-existing conscious level, subsequent encounter
- S06.5X5S – Traumatic subdural hemorrhage with loss of consciousness greater than 24 hours with return to pre-existing conscious level, sequela
S06.5X6 – Traumatic subdural hemorrhage with loss of consciousness greater than 24 hours without return to pre-existing conscious level with patient surviving
- S06.5X6A S06.5X6 – Traumatic subdural hemorrhage with loss of consciousness greater than 24 hours without return to pre-existing conscious level with patient surviving, initial encounter
- S06.5X6D S06.5X6 – Traumatic subdural hemorrhage with loss of consciousness greater than 24 hours without return to pre-existing conscious level with patient surviving, subsequent encounter
- S06.5X6S S06.5X6 – Traumatic subdural hemorrhage with loss of consciousness greater than 24 hours without return to pre-existing conscious level with patient surviving, sequela
S06.5X7 – Traumatic subdural hemorrhage with loss of consciousness of any duration with death due to brain injury before regaining consciousness
- S06.5X7A – Traumatic subdural hemorrhage with loss of consciousness of any duration with death due to brain injury before regaining consciousness, initial encounter
S06.5X8 – Traumatic subdural hemorrhage with loss of consciousness of any duration with death due to other cause before regaining consciousness
- S06.5X8A – Traumatic subdural hemorrhage with loss of consciousness of any duration with death due to other cause before regaining consciousness, initial encounter
S06.5X9 – Traumatic subdural hemorrhage with loss of consciousness of unspecified duration
- S06.5X9A – Traumatic subdural hemorrhage with loss of consciousness of unspecified duration, initial encounter
- S06.5X9D – Traumatic subdural hemorrhage with loss of consciousness of unspecified duration, subsequent encounter
- S06.5X9S – Traumatic subdural hemorrhage with loss of consciousness of unspecified duration, sequela
With early treatment of these injuries, patients will have better chances of full recovery. The speed of recovery often depends on the type and extent of damage the hematoma has caused to the brain. It is estimated that only 20-30 percent of people can expect to see a full or nearly full recovery of brain functioning. Even after the treatment for subdural hematoma, many patients are left with some long-lasting problems like mood swings, memory/concentration problems, seizures, speech problems and weakness in limbs. In some cases, there are chances that the symptoms may come back and hence surgery to drain the hematoma may need to be repeated.
Medical coding for subdural hematoma can be complex. By outsourcing medical coding to a reliable medical billing and coding outsourcing company (that provides the services of AAPC-certified coding specialists), healthcare practices can ensure correct and timely medical billing and claims submission.
Nguồn: https://vuihoctienghan.edu.vn
Danh mục: Info








